May 23, 2021
CHENNAMADHAVUNI DIVYA, 8th semester
Roll number-21
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from an available global online community of experts to solve those patients clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Following is the view of my case:
Date of admission :5-5-2021
Chief complaints :
A 38 year old male patient has come to the opd with the chief complaints of
- Fever : since 4 days
- Shortness of breath :since 1 day
- Loss of taste sensation :since 4 days
- Generalized weakness :since 4 days
History of present illness :
Patient was apparently asymptomatic 4 days back and then he developed ,
Fever ,which was insidious in onset ,high grade ,continuous in nature and not associated with chills and rigors.
he had loss of taste sensation.
he had generalized weakness, which was insidious in onset, gradually progressing in nature.
he developed shortness of breath GRADE = 3 of( NYHA classification) a day ago which was, insidious in onset and gradually progressing
he also had a history of loose stools for a day
he had no complaints of: cough, loss of smell, vomitings , nausea ,chest pain
History of past illness :
Not a known case of Diabetes ,hypertension ,asthma ,tuberculosis ,epilepsy ,CVA
No significant surgical history
No known allergic history
Personal history :
Diet - mixed
Appetite - decreased
sleep - adequate
Bowel and Bladder movements - regular
Addictions - drinks wine on a regular basis,
chews tobacco
Drug history :
Insignificant
Family history :
No significant family history
General examination :
Patient is conscious ,coherent ,cooperative and was well oriented to time ,place and person
at the time of examination
he is examined in a well lit room, with consent taken
he is moderately built and well nourished
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
lymphadenopathy - absent
Edema - absent
Vitals : on the day of admission (5/5/2021)
Temperature -98 degrees F
Pulse rate - 96 bpm
Respiratory rate - 20 cpm
Blood pressure - 110/70 mmHg
SpO2 -89% on Room air
GRBS - 110 mg/dl
Day 2 -6/5/2021 :
Pulse rate - 96 bpm
Blood pressure - 140/100 mmHg
SpO2 -89% on room air
96% on 5 liters of O2
GRBS - 111 mg/dl
Day 3 -7/5/2021
Temperature - 98 degrees F
Pulse rate - 84 bpm
Blood pressure - 100/70 mmHg
SpO2 -96% on room air
GRBS - 179 mg/dl
Day 4 - 8/5/2021 (on the day of discharge)
Temperature - 98 degree F
Pulse rate -88 bpm
Blood pressure -120/70 mmHg
SpO2 - 96% on room air
Systemic examination :
CVS : S1 and S2 heart sounds heard
NO murmurs and thrills
RESPIRATORY SYSTEM : Bilateral air entry present position of trachea - centrall
Vesicular breathsounds heard
CNS : intact
ABDOMEN : Soft and non tender
No palpable masses
Bowel sounds heard
NO organomegaly
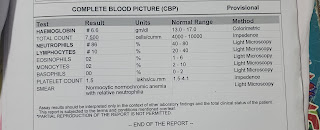
Investigations :
LFT:
Total bilirubin -1.98 mg/dl
Direct bilirubin -0.61 mg/dl
AST -61 IU/L
ALT -41 IU/L
ALP -178 IU/L
Total proteins - 6.4 gm/dl
Albumin -3.6 gm/dl
A/G ratio -1.29
RFT:
Urea - 29 mg/dl
Creatinine -0.4 mg/dl
Uric acid -7.6 mg/dl
Calcium - 9.4 mg/dl
Sodium - 137 mEq/L
Potassium -3.8 mEq/L
Chloride -97 mEq/L
D-Dimer: 100 ng/dl
Serum LDH: 595 units/lit
CRP: 2.4 mg/dl (positive)
Ferritin - >1500 ng/ml
CXR
Provisional Diagnosis :
Viral pneumonia secondary to COVID-19
Treatment :
From 6/5/2021 to 18/5/17 :
- O2 supplementation
- Nebulisation with Budecort ,Duolin- 8th hourly, mucomist - 12th hourly
- Syrup. Grilinctus -10ml/ TID
- Tab. PARACETAMOL 650 mg/PO/OD
- Tab. PANTOP 40 mg/PO/OD
- Temperature charting 6th hourly
- BP, PR, SpO2 monitoring
- IVF- 1 unit NS,1 unit DNS with Optineuron at the rate of 75 ml/hr
- INJ. DEXAMETHASONE 6 mg/IV/OD
- INJ. CLEXANE 40 mg/SC/OD
The patient was advised to discharge on 18/5/2021 ,3.00pm as his condition was stable, with SpO2- 96% on room air and is asked to take the following medications at home,
- Tab. MVT OD for 2 weeks
- Tab. LIMCEE BD for 2 weeks
- Tab. PAN TOP 40 mg OD,30 min before having breakfast
- Tab. PARACETAMOL 650 mg SOS
- Review SOS in case of High-grade fever, breathlessness.
I would like to thank Dr.Rakesh Biswas sir for this oppurtunity and Dr.charan sir for the guidance
Questions:
1. Why are his ferritin levels so high? Is that related to his ,being infected with COVID-19 condition?
2.why is optineuron given to COVID-19 patients? Is
vitamin-B12 deficiency a risk factor for covid?
3.His GRBS shooted to 179 mg/dl, is that because of the COVID-19 infection?


Comments
Post a Comment