- Bilateral pedal edema since 5 months.
- shortness of breath since one months.
- facial puffiness since one month.
History of present illness :
Patient was apparently asymptomatic 5 months back and then he developed ,
Bilateral pedal edema since 5 months.
facial puffiness since one month .
He developed shortness of breath GRADE = 3 to GRADE =4 of( NYHA classification) which was, insidious in onset (ever since he was put on dialysis according to him) and gradually progressing in nature.
He had Fever yesterday ,which was insidious in onset ,high grade ,on and off in nature and associated with chills and dry cough.
He has pain on the right side of the chest,
Onset - sudden
Duration -since 4-5 days.
Type - pricking
Aggrevated on sleeping on the side effected, touching the site of pain .
Relieved on sitting position ,not associated with swelling and tenderness.
He had no complaints of: Loss of smell, vomitings , nausea ,chest pain, no decreased urine output.
History of past illness :
Patient underwent 5 sessions of hemodialysis on CRF past month and is not on hemodialysis since 8 days.
known case of hypertension since 4-5 years and he is on anti hypertensives, does not take his medications regularly.
Diagnosed with CkD ,1 and half year back and was on medications for 6 months which were stopped later with no valid reason.
He was diagnosed with COVID-19 5 months back ,was on home isolation and tested positive in a week, developed bilateral pedal edema since then.
Not a known case of Diabetes ,asthma ,tuberculosis ,epilepsy ,CVA
Has a history of blood transfusion.
No significant surgical history
No known allergic history
Personal history :
Diet - mixed
Appetite - decreased
sleep - adequate
Bowel and Bladder movements - regular
Addictions - drinks alcohol on a regular basis, decreased since 2 years.
chews tobacco on a regular basis, decreased since 2 years.
Drug history :
Nimodipine 10 -20 mg since 1 and half year.
Family history :
No significant family history
General examination :
Patient is conscious ,coherent ,cooperative and was well oriented to time ,place and person
at the time of examination
He is examined in a well lit room, with consent taken.
He is moderately built and well nourished.
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
lymphadenopathy - absent
Pedal edema - present
Vitals : on the day of admission (21/8/2021)
Temperature - 102degrees F
Pulse rate - 105 bpm
Respiratory rate - 40 cpm
Blood pressure - 170/100 mmHg
SpO2 - 85-88% on Room air
Patient was shifted to hemodialysis in the morning( 10:00AM) with UF = 2 liters target.
Patient's SBP shooted to 230/130 mmHg half n hour after starting the dialysis and he was in Acute cardiogenic pulmonary edema and distress of diaphoresis.
He was tachyapneic with RR- 60cpm
SPo2: 75-78 on room air and was connected to high flow O2 (10-12 lit).
Hemodialysis subtypes has been changed to isolate 1.5 lit.
Nebulization with spravent and budecort -STAT
Inj. Nitroglycerine 5ml =5mg ,3ml IV bolus given over 2 minutes
Inj. carix 80mg / IV / STAT.
Inj. Avil 2u / IV / STAT.
Inj. Hydrocortisone 100mg /IV / STAT.
Inj. Neomal 1g / IV / STAT.
Inj. Nitroglycerine one more dose 2ml IV Bolus was given - patient was still tachyapneic with RR: 40 cpm, on high flow O2 (10-12 lit)- SP02 : 90-92 % and 84-88 % on room air.
Inj. Nitroglycerine (2 amp in 40ml 5% D) started with 3ml/hour ,50 micrograms /min -dose ,increased and decreased according to the SBP levels.
Inj. Labetalol 20mg / IV Bolus given over 5 min,
BP : 200/100 mmHg
PR : 172 bpm
After which patient was started on NIV Bipap with in V/O falling sats
SPo2 : 95-98%
Respiratory system ; crackles decreased bilaterally only in basal areas.
Tab. Nifedipine 20 mg / Po / STAT
Tab. Arlcamine 0.1mg / Po / STAT
Hemodialysis was continued for 2 hours.
Patient was shifted back to ICU at 2:00 Am
He was connected back to NIV overnight .
One more dose of Tab. Nifedipine 20 mg / Po / STAT
Tab. Arlcamine 0.1mg / Po / STAT, given at 3:00 Am as,
SBP : 180/100 mm Hg
PR : 100 bpm
Day 2 -22/8/2021 :
Pulse rate - 90 bpm
Blood pressure - 170/100 mmHg
Acute pulmonary edema resolved.
Day 15 -5/9/2021
Pulse rate - 115 bpm
Blood pressure - 190/110 mmHg
SpO2 -92% on Bipap with 15 lit of oxygen.
GRBS - 140 mg/dl
Respiratory system : Inspiratory crepts heard in right axillary and infra axillary areas.
Systemic examination :
CVS : S1 and S2 heart sounds heard
NO murmurs and thrills
RESPIRATORY SYSTEM : Bilateral air entry present position of trachea - centrall
Vesicular breathsounds heard
bilateral crackles heard in all the areas
CNS : intact
ABDOMEN : Soft and non tender
No palpable masses
Bowel sounds heard
NO organomegaly
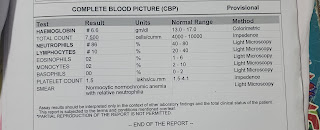
Investigations :
On the day of admission (21-8-21)
complete blood picture
Serum electrolytes
Serum creatinine
Blood urea
APTT
Prothrombin time (PT)
Blood grouping
Serum iron
On day 2 of admission (22-8-21)
Complete blood picture
Interpretation - normal?
On day 3 of admission (23-8-21)
Ultrasound report
Complete blood picture
Blood parasites
ABG
HIV 1/2 Rapid Test
HBsAg - Rapid
Provisional Diagnosis :
CKD(Chronic kidney disease) on Maintenance hemodialysis.
Anaemia of chronic disease.
Treatment :
On day 2 of admission (22-8-21)
On day 3 of admission (23-8-21)
On day 5 of admission (25-8-21)



























Comments
Post a Comment