june 4, 2021
Chennamadhavuni Divya , 8th semester
Roll number - 21
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients’ clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centred online learning portfolio and your valuable inputs on comment box is welcome
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
Following is the view of my case :
Date of admission : 31-5-2021
Chief complaints - A 60 year old female came to the OPD with the chief complaints of,
- Pain in the abdomen since 1 day
- loose stools since 1 day (yesterday morning)
- Vomitings since 1 day (yesterday morning)
History of present illness -
Patient was apparently asymptomatic 2 days back ,then she started having ,
Loose stools - since yesterday morning ,which is sudden in onset, 10 episodes per day , watery in consistency, foul smelling ,non bilious ,non blood stained.
Severe pain in the abdomen - since 1 day ,which is insidious in onset ,gradually progressing and aggravating on food intake with no relieving factors.
Vomitings - 1 episode yesterday morning which was non bilious and non projectile with food particles in the content.
On 31/5/21 (on the day of admission) she was put on nasogastric intubation(ryles tube)and later ,on removal of the ryles tube on 3/6/21 (day 4 of admission) ,billious vomitings and billious stools were noticed.
Giddiness -since morning (on 31/5/21).
She even complaints of burning sensation in the chest .
There are no complaints of fever , burning micturition but decrease in urine output is seen.
She got admitted outside and was given IV fluids and antibiotics yesterday night but her loose stools did not subside ,then she was referred to our hospital.
History of past illness -
She is a k/c/o hypothyroidism since 1 year.
She has a history of renal stones 2 years ago and had lower back ache(LBA )which was subsided on medication.
She underwent hysterectomy 20 years ago.
Not a k/c/o diabetes , hypertension ,coronary artery diseases , tuberculosis , asthma , epilepsy.
Personal history -
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder movements - irregular bowel (loose stools), regular bladder movements.
Addictions - no addictions
Allergies - no known allergies
Family history - not significant
Drug history - She has a history of NSAID abuse 2 months ago.
she has been using Thyronorm 12.5mcg since a year for her hypothyroidism.
General examination -
Patient is conscious , coherent ,cooperative and well oriented to time place and person at the time of examination.
She is examined in a well lit room.
Pallor - absent
Icterus - absent
Clubbing - absent
Cyanosis - absent
Lymphadenopathy - absent
Oedema - absent
VITALS : on 1/6/21 (on day 2 of admission)
Temperature - afebrile
Pulse rate (PR) - 90 beats per min
Blood pressure (BP) -80/60 mmHg
Her BP raised to 90/60 mmHg on administering 4ml NORAD inj.
on 2/6/21 (on day 3 of admission)
Temperature - afebrile
Pulse rate (PR) - 82 beats per min
Blood pressure (BP) -100/60 mmHg
on 3/6/21 (on day 4 of admission)
Temperature - afebrile
Pulse rate (PR) - 80 beats per min
Blood pressure (BP) -110/70 mmHg
on 4/6/21 ( on day 5 of admission)
Temperature - afebrile
Pulse rate (PR) - 90 beats per min
Blood pressure (BP) -120/80 mmHg
Systemic examination -
CVS: S1 and S2 heard
No added thrills, murmurs
RESPIRATORY SYSTEM: Normal vesicular breath sounds heard
Bilateral air entry present.
PER ABDOMEN: soft , distended , Tenderness -diffuse (present all over the abdomen) and rebound tenderness in the lower abdomen is present.
- Abdominal guarding - present
- Bowel sounds -not heard
- Abdominal girth - 97cm
- No palpable masses.
PER RECTAL : Decreased sphincter tone
- No palpable masses.
- Mucoid stained glove fingers.
CNS: intact
Investigations -
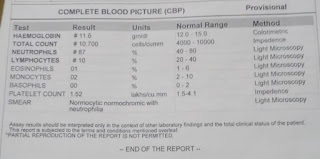
Complete blood picture (CBP) : 31/5/21 ( on the day of admission)
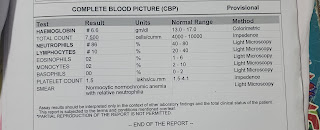
4/6/21 (on 4th day of admission )
Complete urine examination (CUE) : 1/6/21 (on day 2 of admission)
Serum creatinine : 1/6/21 ( on day 2 of admission)
Serum electrolytes : 1/6/21 ( on day 2 of admission)
ABG : 1/6/21 ( on day 2 of admission) Interpretation - metabolic acidosis
Stool examination : bacterial culture and sensitivity report
3/6/21 ( on day 4 of admission)
Liver function test (LFT) : 1/6/21 ( on day 2 of admission)
Renal function test ( RFT) : 4/6/21 ( on day 5 of admission)
ECG :
USG ABDOMEN done on 1/6/21 ( on day 2 of admission) impression :
- Dilated fluid filled small bowel loops are noted with sluggish or absent peristalsis with maximum diameter of 3.5 cm - small bowel obstruction.
- Mild ascitis is seen.
- Oedematous and collapsed ascending colon and caecum, with circumferential wall thickening - suggesting infective /inflammatory etiologies.
- Fatty liver is seen.
Ultrasound report form :
- Evidence of diffuse abdominal gas being noted.
- NO evidence of free fluid collection in the abdomen and pelvis
In correlation with X-ray erect abdomen and USG features of sluggish to absent peristalsis in the visualised bowel loops, a possibility of intestinal (small bowel) obstruction is considered which is not due to any actual physical (mechanical) compression of the bowel , but because of an infective/inflammatory process.
CE-CT done on 4/6/21 (on day 5 of admission)
Provisional diagnosis - Acute Gastroenteritis with paralytic ileus.
Treatment - on 31/5/21 (on day 1 of admission)
RX.
1. Inj. PANTOP 40mg IV/BD
2. Inj. ZOFER 4mg IV/TID
3. Inj. METROGYL 500mg /IV/TID
4. Inj. MONOCEF 1gm/IV/BD
5. IVF - 2 units of NS and RL - at the rate of 100ml/hr
6. Tab. THYRONORM 12.5 micrograms PO OD
7. BP / PR / Temperature / SpO2 - 4th hourly
8. Strict I/O charting
on 1/6/21 (on day 2 of admission)
1. Inj. PANTOP 40mg IV/OD
2. Inj. ZOFER 4mg IV/TID
3. Inj. METROGYL 500mg /IV/TID
4. Inj. MONOCEF 1gm/IV/BD
5. IVF - 2 units of NS , RL and DNS - at the rate of 100ml/hr
6. Tab. THYRONORM 12.5 micrograms PO OD
7. BP / PR / GRBS - 4th hourly
8. Strict I/O charting
on 2/6/21 (on day 3 of admission)
1. Inj. PANTOP 40mg IV/BD
2. Inj. ZOFER 4mg IV/TID
3. Inj. METROGYL 500mg /IV/TID
4. Inj. MONOCEF 1gm/IV/BD
5. IVF - 2 units of NS , RL and DNS - at the rate of 100ml/hr
6. Tab. THYRONORM 12.5 micrograms PO OD
7. BP / PR / GRBS - 4th hourly
8. Strict I/O charting
9. Abdominal girth measurement
10. Tab. SPORLAC- DS TID
11. Tab. DORTIN- M PO SOS
12. Cap AD -100 PO BD
on 3/6/21 (on day 4 of admission)
1. Inj. PANTOP 40mg IV/BD
2. Inj. ZOFER 4mg IV/TID
3. Inj. METROGYL 500mg /IV/TID
4. Inj. MONOCEF 1gm/IV/BD
5. IVF - 2 units of NS , RL and DNS - at the rate of 100ml/hr
6. Tab. THYRONORM 12.5 micrograms PO OD
7. BP / PR / GRBS - 4th hourly
8. Strict I/O charting
9. Abdominal girth measurement
10. Tab. SPORLAC- DS TID
11. Tab. DORTIN- M PO SOS
12. Cap AD -100 PO BD
on 4/6/21 (on day 5 of admission)
1. Inj. PANTOP 40mg IV/BD
2. Inj. ZOFER 4mg IV/TID
3. Inj. METROGYL 500mg /IV/TID
4. Inj. MONOCEF 1gm/IV/BD
5. IVF - 2 units of NS , RL and DNS - at the rate of 100ml/hr
6. Tab. THYRONORM 12.5 micrograms PO OD
7. BP / PR / GRBS - 4th hourly
8. Strict I/O charting
9. Abdominal girth measurement.
The current update of the case -
On 4/6/21 she has been taken for EXPLORATIVE LAPAROTOMY.
Aspirate collected after opening the abdomen
Post hysterectomy scar adhesion
Repair of the serosal tear
Thank you Rakesh Biswas sir, for the opportunity.
Thank you P.Raghu Ram sir and Sai Charan sir for the guidance.

















Comments
Post a Comment