August 31st, 2021
CHENNAMADHAVUNI DIVYA, 9th semester
Roll number-21
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from an available global online community of experts to solve those patients clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Following is the view of my case:
Date of admission:-28-8-2021
Chief complaints :
A 56-year-old male patient has come to the opd with the chief complaints of,
- Fever since 10 days.
- Shortness of breath since 5 days.
- Cough since 10 days.
- Generalized weakness since 15 days.
History of present illness :
The patient was apparently asymptomatic 15 days back and then he developed,
Generalized weakness, which was insidious in onset and gradually progressing.
Fever which was insidious in onset, high grade, intermittent in nature and associated with chills, rigours,cold,headache,loss of smell and taste sensations.
He developed shortness of breath which was in stage 2 since 15 days and has progressed to stage 4 since 5 days(MMRC classification) ,which was insidious in onset and gradually progressing ,increased on excertion and decreased on rest (supine position).
He has had productive cough which is mucoid in consistency, small in quantity,non-foulsmelling and non-blood stained, associated with pain all over the chest.
He has had joint pains for a year,
Joint pains:
Onset – insidious
Duration -1 year
Gradually progressing, started in the knees and passed on to shoulders, lower back, arms, legs and mildly to his wrists.
Not associated with swelling, tenderness.
Pains are present throughout the day for a year.
Type- dragging
Aggravating factors -work
Relieving factors -not relieved on medications.
Not associated with pedal oedema, facial puffiness, palpitations, decreased urine output etc.
History of past illness :
Not a known case of Diabetes, hypertension asthma, tuberculosis, epilepsy, CVA etc
Surgical history - underwent surgery for renal caliculi 10 years back.
No known allergic history
Personal history :
Diet - mixed
Appetite - decreased
sleep - adequate
Bowel and Bladder movements - regular
Addictions - beedi since 30 years, 1 pack per day.
Alcoholic for 10 years, 90 ml per day.
Drug history :
Diuretics, NSAIDS, multi vitamins ,hydroxychloroquine, steroids and antibiotics .
Family history :
No significant family history
General examination :
Patient is conscious ,coherent ,cooperative and was well oriented to time ,place and person
at the time of examination.
He is examined in a well lit room, with consent taken
He is moderately built and well nourished
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
lymphadenopathy - absent
Edema - absent
Vitals : on the day of admission (28/8/2021)
Temperature -102 degrees F
Pulse rate - 96 bpm
Respiratory rate - 20 cpm
Blood pressure - 90/50 mmHg
Day 2 -29/8/2021 :
Temperature-98.6 degree F
Pulse rate - 92 bpm
Respiratory rate - 22 cpm
Blood pressure - 130/80 mm Hg
SpO2- 96%
GRBS - 132 mg/dl (8:00am) ,189 mg/dl (12:00 pm)
Day 3 -30/8/2021
Temperature - 98 degrees F
Pulse rate - 80 bpm
Blood pressure - 130/70 mmHg
SpO2 -98% on room air (8:00am)
GRBS - 132 mg/dl (8:00am) ,120 mg/dl (8:00 pm)
Day 4 - 31/8/2021
Temperature - 98 degree F
Pulse rate -80 bpm (8:00am)
Blood pressure -120/70 mmHg
SpO2 - 96% on room air (8:00am)
GRBS - 132 mg/dl (8:00am) ,138 mg/dl (2:00 pm)
Day 5 - 1/9/2021
Temperature -afebrile
Pulse rate - 76 bpm
Respiratory rate - 20 cpm
Blood pressure - 100/60 mmHg
SPo2- 98% on room air
Day 6 - 2/9/2021
Temperature -afebrile
Pulse rate - 68bpm
Respiratory rate - 26 cpm
Blood pressure - 130/70 mmHg
SPo2- 91% on room air
Systemic examination :
CVS : S1 and S2 heart sounds heard
NO murmurs and thrills
RESPIRATORY SYSTEM : Bilateral air entry present position of trachea - centrall
Wheeze on inspiration was appreciated
in all the areas.
Bilateral Fine crepitations where heard.
CNS : intact
ABDOMEN : shape of abdomen -obese
Soft and non-tender
No palpable masses
Bowel sounds heard
NO organomegaly
Investigations :
RFT : 28/8/21 (on the day of examination)
Urea - 37 mg/dl
Creatinine -1.3 mg/dl
Sodium - 142 mEq/L
Potassium -3.1 mEq/L
Chloride -104 mEq/L
ABG : 28/8/21 (on the day of examination)
Interpretation : respiratory alkalosis
PH - 7.5
PCo2 - 22.6
Po2 - 51
So2 - 85
HCo3 - 15.7
Random blood sugar : 28/8/21 (on the day of examination) - 123 mg/dl
RT-PCR : 28/8/21 ( on the day of admission)
Chest x-ray: 28/8/21 (on the day of admission)
Interpretation - pulmonary hypertension?
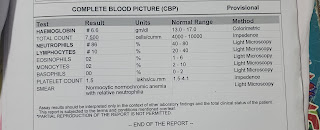
Hemogram: 28/8/21 ( on the day of admission)
Complete urine examination (CUE) : 28/8/21 (on the day of admission)
HBsAG- Rapid : 28/8/21 (on the day of admission)
HIV 1/2- Rapid : 28/8/21 (on the day of admission)
Anti HCV Antibodies : 28/8/21 (on the day of admission)
Blood grouping : 28/8/21 (on the day of admission)
29/8/21 (on day 2 of admission)
Ultrasound report : 29/8/21 (on day 2 of admission)
Review Ultrasound On 30/8/21 : diffuse abdominal tenderness.
Colour doppler 2D Echo : 30/8/21 (on day 3 of admission)
ECG: 28/8/21 ( on the day of admission)
Fever charting :
Bacterial culture and sensitivity reports : 31/8/21 (on day 4 of admission)
Spirometry : 1/9/21 (on day 5 of admission)
Provisional Diagnosis :
Viral pneumonia acute exacerbation of Chronic obstructive pulmonary disease.
Treatment :
28/8/21 : (on the day of admission)
1) Head-end elevated.
2) O2 inhalation to maintain SPo2 > or equal to 94%
3) Inj. Ceftriaxone 1mg Iv/BD
4) Inj. Pantop 40mg Iv/OD
5) Inj. Neomol 100ml Iv/sos ( if the temperature is > or equal to 101° F)
6)Nebulization - with Budecort: 6th hourly
Duolin: 8th hourly
Mucomist: 6th hourly
7)Tab. Paracetamol - 650mg PO/TID
8)Tab. Montex LC - PO/HS
9)BP/PR/RR/Temperature - 4th hourly
29/8/21 : (on 2 day of admission)
1) O2 inhalation to maintain SPo2 > or equal to 94%
2) Inj. Ceftriaxone 1mg Iv/BD
3) Inj. Pantop 40mg Iv/OD
4) Inj. Neomol 100ml Iv/sos ( if the temperature is > or equal to 101° F)
5)Nebulization - with Budecort: 6th hourly
Duolin: 8th hourly
Mucomist: 6th hourly
6)Tab. Paracetamol - 650mg PO/TID
7)Tab. Montex LC - PO/HS
8)BP/PR/RR/Temperature - 4th hourly
30/8/21 : (on 3 day of admission)
1) O2 inhalation to maintain SPo2 > or equal to 94%
2) Inj. Ceftriaxone 1mg Iv/BD
3) Inj. Pantop 40mg Iv/OD
4) Inj. Neomol 100ml Iv/sos ( if the temperature is > or equal to 101° F)
5)Nebulization - with Budecort: 6th hourly
Duolin: 6th hourly
Mucomist: 6th hourly
6)Tab. Paracetamol - 650mg PO/TID
7)Tab. Montex LC - PO/HS
8)BP/PR/RR/Temperature - 4th hourly
31/8/21 : (on day 4 of admission)
1) O2 inhalation to maintain SPo2 > or equal to 90%
2) Inj. Ceftriaxone 1mg Iv/BD
3) Inj. Pantop 40mg Iv/OD
4) Inj. Neomol 100ml Iv/sos ( if the temperature is > or equal to 101° F)
5)Nebulization - with Budecort: 6th hourly
Duolin: 6th hourly
Mucomist: 6th hourly
6)Tab. Paracetamol - 650mg PO/TID
7)Tab. Montex LC - PO/HS
8)BP/PR/RR/Temperature - 4th hourly
1/9/21 : (on day 5 of admission)
1)O2 inhalation to maintain SPo2 > or equal to 90%
2) Inj. Ceftriaxone 1mg Iv/BD
3) Inj. Neomol 100ml Iv/sos ( if the temperature is > or equal to 101° F)
4)Nebulization - with Budecort: 6th hourly
Duolin: 8th hourly
Mucomist: 6th hourly
5)Tab. Paracetamol - 650mg PO/TID
6)Tab. Montex LC - PO/HS
7)Tab. Pulmoclear 600mg PO/BD
8)Tab. Ultracet 1/2-1/2-1/2-1/2
9)Monitor vitals 4th hourly
10)Tab. Pregabalin 75mg P0/HS
11)Tab. MNT PO/OD (2:00 pm)
12)Syp. Grillnictus 5ml PO/TID




















Comments
Post a Comment